Uganda
Malaria Facts
Uganda has made great progress in reducing malaria transmission from 42% in 2009 to 9% in 2018.[1] Despite this, in 2021 Uganda had the 3rd highest global burden of malaria cases (5.1%) and the 7th highest level of deaths (3.2%). [2] It also had the highest proportion of malaria cases in East and Southern Africa of 23 % in 2021.[2]
Between 2020 and 2021, the estimated number of malaria cases remained stable at 284 per 1000 of the population at risk, while deaths fell 6.1% from 0.46 to 0.43 per 1000 of the population at risk over the same period. [2] There is stable, perennial malaria transmission in 95 percent of the country, with Anopheles gambiae s.l. and An. funestus s.l. the most common malaria vectors. [3]
In 2018 there was a lower-than-expected number of malaria cases because there was no seasonal transmission peak between week 20 and 30, and mass distribution of nets was completed in early 2018. In 2019, on the other hand, malaria cases increased in comparison to 2018 as the transmission peak was untypically long due to increased rains and ageing of mosquito nets distributed in 2017/2018. [4] Progress regarding children is promising. Data from the 2018 Malaria indicator survey (MIS) revealed that 4% of children aged 6–59 months were severely anaemic in 2018 versus 6% in 2016. Furthermore, 87% of children with fever were able to seek care in 2018, an increase from 81% in 2016. [3]
To accelerate progress towards global malaria targets, WHO and RBM Partnership has rolled out the High Burden High Impact approach in 10+1 countries which include Uganda.[1] The Uganda Malaria Reduction and Elimination Strategic Plan 2021-2025 aims to reduce malaria infections by 50 percent, morbidity by 50 percent and mortality by 75 percent by 2025. The Plan aims to achieve these goals through stratification to ensure appropriate tailoring of intervention mixes for the various epidemiologic contexts, universal coverage of services (including in the private sector), robust data management and social behavioural change, multisectoral collaboration, and malaria elimination in two districts. [4]
Although the entire population is at various levels of risk, marginalised populations are confronted with economic, social and contextual challenges and barriers that may limit their access to malaria prevention, treatment and control programmes. These populations include vulnerable and underserved populations such as:
- Children under five years and pregnant women
- People living with HIV
- People with disabilities
- Inmates and other detainees
- People in closed/congregate settings
- Migrant and mobile populations
- Internally displaced populations
- Refugees and asylum seekers
- Older persons
- People affected by ethnic, geographical or cultural barriers.
To address the human rights barriers, Uganda has developed a comprehensive strategy document aimed at malaria-free Uganda through protecting human rights, achieving gender equality, and improving health equity for all Ugandans in all their diversity – Leaving no one behind: A national plan for achieving equity in access to HIV, TB and Malaria services in Uganda, 2020-2024. [1]
Malaria transmission
Plasmodium falciparum accounts for 98% of infections; both P. vivax and P. ovale are rare and do not exceed 2% of malaria cases in the country. [3]
The country experiences two malaria transmission types: [3]
- Stable, perennial malaria transmission which exists in 90–95 % of the country
- Low and unstable transmission with potential for epidemics in 5-10% of the country.
Transmission peaks are aligned with the two annual rainy seasons, which take place from March to May and from September to November.[3] To guide the deployment of interventions, the country has been stratified into three strata, based on epidemiologic, entomologic and socio-behavioral characteristics:[1]
- Very low burden areas (<2% malaria prevalence) about 2.4% of the population
- Urban cities (6.2m; 14.4% of total population)
- High burden (rest of the country) areas.
Case management
For severe malaria, intravenous or intramuscular artesunate is the recommended treatment for all adults and children. When artesunate is not available, parenteral artemether or quinine can be used. Once a patient is able to tolerate oral medication, and after at least 24 hours of parenteral therapy, treatment should be completed with a full course of an oral first-line artemisinin combination therapy (ACT).
For pre-referral intervention before transfer to an appropriate level of care, a single intramuscular dose of artesunate, intramuscular artemether, or intramuscular quinine can be used. At the community and lower-level health facilities, or where injections are not available, a single dose of rectal artesunate can be used as pre-referral intervention for children under six years of age only.[3]
Between 2020–22, the total need for injection artesunate is estimated to be 7,002,881 ampules.[1] These are being financed by PMI (700, 288 ampoules) and the Global Fund (6,302,593 ampoules. For pre-referral intervention in suspected severe malaria cases, the total estimated quantity of rectal artesunate is 706,243 suppositories.
Malaria in pregnancy
Uganda has adopted the WHO guidelines for Intermittent preventive treatment in pregnancy (IPTp), which includes a treatment dose of sulfadoxine-pyrimethamine (SP) for HIV negative women at each scheduled antenatal care (ANC) visit starting at 13 weeks gestational age, with a minimum of four weeks between doses, and a recommended minimum of three doses (IPTp3). SP is recommended to be administered as directly observed therapy (DOT).
Between 2016 and 2018, however, the proportion of pregnant women who received two or more doses of intermittent preventive treatment during their last pregnancy (IPTp) in the last two years increased from 46% to 72%, and the proportion who received three or more doses increased from 17% to 41%. [3] In 2018, 83% of households reported having at least one insecticide-treated bednet (ITN). This was an improvement over 2016 (78% of households) although lower than reported in 2014 (90%). Between 2016–2018, there was a slight increase in the use of mosquito nets by pregnant women (64% in 2016, 65% in 2018) and a slight decline in use by children under five years of age (62% in 2016, 60% in 2018); in both cases, usage had declined since 2014 (75% for pregnant women; 74% for children under five years of age). [2]
Seasonal malaria chemoprevention
Uganda’s NMCD does not currently implement seasonal malaria chemoprevention (SMC) to reduce malaria transmission because transmission is not highly seasonal (60% of cases do not occur within a four-month period). However, there is a pilot SMC program in Karamoja region, which has one rainy season unlike the other regions of the country with two rainy seasons.
Malaria Consortium, in collaboration with NMCD, is carrying out the pilot with funding from GiveWell. The study team has indicated that SMC with sulfadoxine-pyrimethamine + amodiaquine (SPAQ) could potentially provide benefits in Uganda where there is relatively high prevalence of resistance to SP.
Insecticide-treated nets
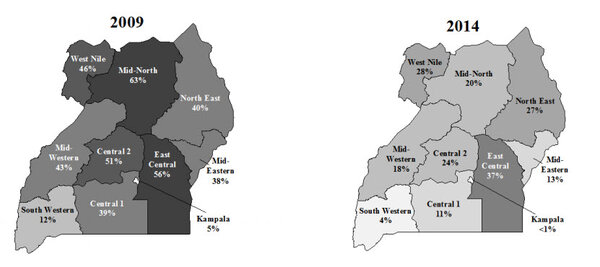
Ownership of at least one ITN has generally increased over time. Households owning at least one ITN increased from 47% in 2009 to 83% in 2018–2019. Full household ITN coverage, as measured by the percent of households with at least one ITN for every two people in the household, increased from 16% in 2009 to 54%in 2018–2019.[3] Uganda conducted a mass ITN coverage campaign from June 2020 to March 2021. The ITN ownership (households owning at least one ITN) levels nationally were estimated to increase to at least 90%.[3]
ITN use by children increased from 33% in 2009 to 60 % in 2018–2019. Use of ITNs by pregnant women increased from 44% in 2009 to 65%in 2018–2019. However, between 2016 and 2018–2019, there was a slight decline in ITN use among children under five years of age over the same period (62% to 60%).[3]
Gender disparities
Gender-based disparities and social customs have created hurdles for accessing malaria related services. A key example of this is that health seeking decisions are often taken by male family heads of family and this could lead to delays in seeking treatment. In addition, there are instances where only men are sleeping under ITNs at the expense of children or pregnant women. Steps to tackle these challenges include attainment and maintenance of universal coverage of bed nets. [5]
Survey data also reveals that severe anaemia (mostly due to malaria) continues to be a public health problem in Uganda. [6] For severe malaria in pregnancy, intravenous artesunate is recommended as the first-line treatment and quinine as the alternative. [2] All malaria in pregnancy cases are noted in antenatal care registers and reported in health management information system platforms such as District Health and Information Systems databases. [2] The Integrated Management of Malaria curriculum includes management of uncomplicated and severe malaria, management of malaria in pregnancy, and parasite-based diagnosis with rapid diagnostic tests or microscopy, including how to manage a patient with fever and a negative rapid diagnostic test (RDT) or microscopy result.[2]
The World Health Organisation’s Global Malaria Programme has developed an easily adaptable repository structure in District Health Information Systems [6], with guidance on relevant data elements and indicators, their definitions and computation to cover key thematic areas. So far, work to develop these databases has started in the Gambia, Ghana, Mozambique, Nigeria, Uganda and the United Republic of Tanzania. [6]
Malaria Training
Health workers at all levels (including the private sector) were trained in integrated management of malaria (IMM) in 102 of 112 districts (10,500 HWs), including training in the management of severe malaria. Clinical audits for severe malaria were performed in 34 of 112 districts.
Severe malaria policy and practice
| Recommendation | Treatment |
|---|---|
| Strong | IV artesunate |
| Alternative | IV quinine |
| Alternative | IM artemether |
| Recommendation | Pre-referral |
|---|---|
| Strong | Rectal artesunate |
| Alternative | IM quinine |
* During the first trimester pregnancy, the most effective anti-malarial medicine should be used under medical supervision as the major objective in treatment of severe malaria is to prevent death.
Market information