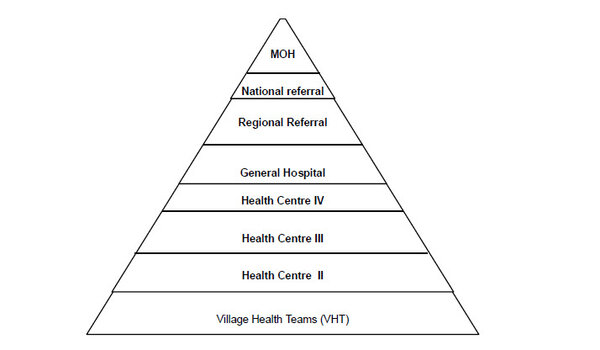
Uganda health system

Health services structure:
National Referral Hospitals
Regional Referral Hospitals
General hospitals
Health centres (HCs) IVs, IIIs, IIs, and Is
HC IV
- Health sub-district
- Day-to-day management and technical oversight of the lower level health facilities
- Leadership in the planning and management of health services including supervision and quality assurance
- Provision of technical, logistical and capacity development support to the lower health units and communities including procurement and supply of drugs.
HC III
- Provide basic preventive and curative care
- Provide supportive supervision to the community and HC IIs under their jurisdiction
HC II
- Provide first level of interaction between the formal health sector and the communities
- Provide outpatient care, community outreach services, and nurses provide comprehensive services and linkages with the Village Health Team (VHT)
HC I
- No physical structure but a team of people—VHTs—that link health facilities with the community
- VHT networks facilitate health promotion, service delivery, and community participation in access and utilization of health services
- 2015 assessment by MoH showed the VHT strategy has been implemented to varying degrees across the districts
Défis
Challenges
HC I
- Capacity to coordinate, train, and supervise VHT activities at district level
- Funding
- High attrition among VHTs due to lack of tools, resources, motivation, and regular supervision
- Coordination and supervision by the MoH
Private sector
The private sector is the preferred first point of contact for nearly 59% of children with fever, with 44% going to private hospitals or clinics and 14 percent going to private pharmacies.[3] The private sector’s contribution to service delivery has been lacking in coordination, fragmented, and difficult to measure. Moreover, the midterm review of the previous national malaria strategy indicated minimal adherence to national malaria policies and guidelines in the private sector. The Uganda Malaria Reduction and Elimination Strategic Plan’s (UMRESP’s) second strategic objective seeks to improve efficiency of service delivery coordination, information management, and sustainability of the private sector for health, and will deploy four strategies to achieve this:
- Establish a malaria private sector coordination mechanism to strengthen the coordination, advocacy, and resource mobilisation capacity of the private sector, and support information gathering and sharing among private sector actors regarding malaria interventions.
- Strengthen the capacity of the private sector to deliver quality malaria preventive and curative services by training and mentoring private sector health workers in integrated malaria management using appropriate modalities, increasing their access to affordable, quality assured malaria commodities and conducting quality assurance for malaria diagnostics.
- Strengthen the private sector accreditation and regulatory environment, including data reporting, through private sector service providers mapping, capacity-building, incentives and disincentives to conform to good practice norms, and to increase participation in research, evaluation, and decision fora.
- Ensure sustainable financing of affordable malaria interventions at workplaces and institutions through supporting the implementation of public–private partnerships for health strategic arrangements. The NMCD also aims to leverage the private sector to optimise coverage by health insurance providers, enhance uptake and use of market shaping and subsidised access strategies, and increase engagement in corporate social responsibility for malaria control.